Acute Zonal Occult Outer Retinopathy (AZOOR)
What Causes AZOOR?
The cause of AZOOR is unknown, although it is thought to be related to an auto-immune process whereby the individual’s immune system damages the outer or peripheral retinal cells. Further studies are needed, however, to clarify the mechanisms of this disease.
What Are the Symptoms of AZOOR?
Patients may notice a sudden onset of scotoma (an area of the visual field that is blurry or missing, like a blind spot) or blurred vision, often accompanied by photopsia (flashing or shimmering lights) in the vision. Some patients may note a history of a recent viral-like illness in the weeks preceding the onset of visual symptoms. Usually, one eye is affected, but the other may also become involved.
Who Gets AZOOR?
AZOOR typically affects women more commonly than men – almost three times more. Often, patients are myopic or nearsighted. The average age at diagnosis is in the 30s, although younger and much older patients have also been diagnosed with this condition. Caucasian persons are more commonly affected than other ethnic groups.
How Does AZOOR Affect the Eyes?
Photoreceptor Degeneration
AZOOR is thought to affect vision by causing degeneration of photoreceptors in a specific “zone” of the retina – thus the term “zonal” in the name. The retina is the thin nerve tissue that lines the back wall of the eye to receive light signals from the outside world. If the eye were a camera, the retina would be the camera’s film.
The photoreceptors are the cells in the outermost part of the retina that first receive and process these light signals – thus the term “outer retinopathy” in AZOOR’s name.
Some Facts about the Retina
The retina is the light-sensitive tissue that lines the inside surface of the eye.
The retina contains photoreceptor cells that convert (or process) incoming light into electrical impulses. These electrical impulses are carried by the optic nerve (which resembles your television cable) to the brain, which finally interprets them as visual images.
There are two types of photoreceptors: rods and cones, the light-processing cells responsible for peripheral (side) and central (straight-ahead) vision.
Rods:
- The specialized, highly light-sensitive retinal processing cells can function in low light levels. They provide peripheral (or side) vision, are responsible for dark adaptation, and are most sensitive to movement/motion. They are less sensitive to color perception.
- A normal retina contains approximately 120 million rods, primarily in the peripheral or outer retina.
- Rods provide scotopic vision, which refers to eyesight in low-light conditions.
Cones:
- The specialized retinal processing cells function in bright light levels and provide central (or straight-ahead) vision, sharp visual acuity, detail, and color vision. They require bright light to function and are not sensitive to lower light levels.
- A normal retina contains approximately 6-7 million cones, primarily in the macula, the small area in the retina’s center that provides clear central vision. Cones are the most concentrated in the fovea, located in the center of the macula, and provide the sharpest detail vision.
- Cones provide photopic vision, which refers to eyesight in daylight conditions.
Visual Acuity
Visual acuity (the measurement of the sharpness or clarity of the vision in each eye, using the letter chart) is often minimally affected, with almost half of the patients exhibiting vision of 20/20 or better. However, some patients may have a significant decrease in vision.
Reduced Visual Fields
In AZOOR, abnormalities in the retina can result in a visual field defect. A variety of visual field defects have been noted. Visual field testing can draw a map of the visual fields and show where the patient may have lost vision, mainly peripheral (or side) vision.
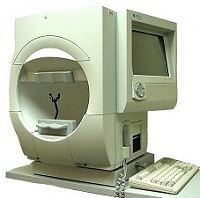
- The most commonly used visual field test is the Humphrey Field Analyzer (pictured at right). The part that the patient uses for testing resembles a large bowl. One eye is covered, while the other remains stationary and focused on a central point. At the same time, small white lights of varying sizes and intensities flash at different locations around the bowl.
- The patient is instructed to press a button whenever they see a flashing light. Recording which lights the patient does and does not see creates a visual field map.
- Based on the responses, this test can determine if there are “visual field defects” or areas of the visual field which the eye is not seeing (like a blind spot) due to an abnormality in the retina, the optic nerve that transmits visual signals from the brain to the retina, or the parts of the brain that transmit or process the visual information.
Diagnosing AZOOR
On examination of the eye, AZOOR can be very difficult to diagnose because the clinical appearance of the eye and the retina may be fairly normal.
- Some changes that may be noted include initial subtle changes in the retinal pigment epithelium (a layer of cells that sits adjacent to, and nourishes, the photoreceptors of the retina) to more significant retinal pigment epithelial abnormalities or changes in the retinal vessels in that area.
- There may be some changes in the pigmentation surrounding the optic nerve (the cable connecting the retina to the brain to transmit the light signal). Some patients may have inflammatory cells visible in the vitreous. An optical coherence tomography (OCT) scan, which uses light to take cross-sectional retina images and visualize individual cell layers in the retina, may show zones of outer retinal and photoreceptor layer degeneration.
- A photograph called a fundus autofluorescence may be taken, in which the retina’s natural fluorescence [i.e., the emission of light or other radiation] is visualized. Abnormalities in this can be seen in AZOOR due to the damaged retinal pigment epithelial cells, which house a highly fluorescent substance captured in these images.
- Additional testing may be performed, such as fluorescein angiography or indocyanine green angiography. This involves the injection of a vegetable-based dye or iodine-based dye into the arm. The dye traverses the blood and reaches the eye approximately 10 seconds later, then moves through the retinal blood vessels. Various abnormalities in these tests may also suggest a diagnosis of AZOOR.
What is the Natural Course of AZOOR?
- Some patients may notice an early progression in the visual field loss, but this often stabilizes eventually, usually by six months.
- Up to 25% of patients may have a variable improvement in the visual field.
- As noted above, visual acuity is usually not significantly affected, although some patients can have a profound decrease in visual acuity.
- Some patients (fewer than 25%) may have recurrences of AZOOR at a later date.
How is AZOOR Treated?
A number of treatments have been tried with this condition, including steroids and other immune suppression therapies (due to the thought that the condition is caused by an auto-immune mechanism), though none have demonstrated high efficacy. Research in this area is ongoing.
By Mrinali Patel Gupta, M.D.