¿Cuáles son los distintos tratamientos para el glaucoma?
El glaucoma es una enfermedad crónica que debe vigilarse de por vida. Con un seguimiento adecuado y el cumplimiento del tratamiento, el glaucoma puede controlarse a fin de minimizar cualquier limitación de la visión o del estilo de vida.
Los análogos de la prostaglandina
Los análogos de la prostaglandina son los colirios más recetados. La prostaglandina es una proteína natural de la sangre que puede reducir la presión intraocular (dentro del ojo) y que tiene muchos otros efectos terapéuticos. “Análogo” significa que el fármaco es comparable o similar a la prostaglandina, pero tiene una composición química algo diferente.
Por lo tanto, los análogos de la prostaglandina (AGP) son fármacos que se utilizan para tratar el glaucoma de ángulo abierto o la hipertensión ocular. Estos medicamentos aumentan el flujo de salida o drenaje del humor acuoso del ojo y así reducen la presión intraocular.
Algunos de los AGP más comunes son los siguientes:
- Travatan (nombre genérico: travoprost);
- Xalatan (nombre genérico: latanoprost);
- Lumigan (nombre genérico: bimatoprost);
- Zioptan (nombre genérico: tafluprost).
Los inhibidores de la anhidrasa carbónica
Los inhibidores de la anhidrasa carbónica son sustancias farmacéuticas que reprimen la acción de la anhidrasa carbónica, una enzima que desempeña una función crucial en la regulación del pH y los niveles de líquido corporal. Los inhibidores de la anhidrasa carbónica reducen la absorción de iones de bicarbonato en el organismo y disminuyen la absorción de sal, lo que reduce los niveles de líquido corporal.
Por lo tanto, los inhibidores de la anhidrasa carbónica (IAC) disminuyen la presión ocular al reducir la producción de líquido del propio ojo.
Estos medicamentos incluyen los siguientes:
- Trusopt (nombre genérico: clorhidrato de dorzolamida);
- Azopt (nombre genérico: brinzolamida).
Si se necesita medicación adicional a fin de controlar la presión ocular, también se recetan inhibidores de la anhidrasa carbónica en formato líquido o en pastillas. Estos medicamentos líquidos incluyen los siguientes:
- Diamox (nombre genérico: acetazolamida);
- Neptazane (nombre genérico: metazolamida).
También puede recetarse en forma de pastillas a las personas que no toleran los colirios.
Los agonistas alfaadrenérgicos
Estos fármacos disminuyen la presión intraocular al reducir la producción de humor acuoso y al aumentar el flujo de salida del líquido.
Estos medicamentos incluyen los siguientes:
- Alphagan (nombre genérico: tartrato de brimonidina);
- Iopidine (nombre genérico: clorhidrato de apraclonidina).
Los bloqueadores adrenérgicos beta
Estos fármacos reducen la producción de humor acuoso y, por lo tanto, la presión intraocular. Se los suele tolerar bien y son eficaces. Sin embargo, los médicos los evitan en caso de que presente asma o una frecuencia cardíaca lenta (bradicardia).
Estos medicamentos incluyen los siguientes:
- Timoptic (nombre genérico: maleato de timolol);
- Betimol (nombre genérico: hemihidrato de timolol);
- Betagan (nombre genérico: clorhidrato de levobunolol);
- Betoptic (nombre genérico: clorhidrato de betaxolol);
- Ocupress (nombre genérico: carteolol).
Los fármacos combinados
Los fármacos combinados integran dos medicamentos en una formulación, entre ellos se encuentran los siguientes:
- Cosopt (combinación de clorhidrato de dorzolamida y maleato de timolol);
- Combigan (combinación de tartrato de brimonidina y maleato de timolol);
- Simbrinza (combinación de brinzolamida y tartrato de brimonidina).
Los colores de las tapas de los frascos
Si utiliza más de un tipo de colirio, es posible que deba administrar cada medicamento en un orden determinado. Puede utilizar el color de la tapa del frasco para llevar la cuenta de cada tipo de colirio:
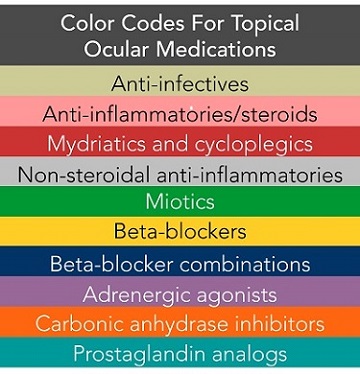
- Los análogos de la prostaglandina tienen tapas de color turquesa.
- Los inhibidores de la anhidrasa carbónica tienen tapas de color naranja.
- Los agonistas alfa-adrenérgicos tienen tapas de color morado.
- Los bloqueadores adrenérgicos beta tienen tapas de color amarillo o azul.
- Los medicamentos combinados suelen tener tapas de color azul.
Cumplir el régimen de medicación oftalmológica
Si le diagnosticaron un glaucoma, es fundamental que siga el régimen de medicación ocular que el oftalmólogo recetó. Con el objetivo de que la medicación reduzca la presión intraocular de manera eficaz, es esencial seguir a diario el régimen de colirios recetados.
A veces, el cumplimiento puede ser difícil porque administrar los colirios puede resultar molesto.
Un consejo para este problema es refrigerar las gotas. Al refrigerarlas, las gotas estarán frías y administrarlas se sentirá relajante. Otra ventaja de refrigerar las gotas es que sentirá cuando entran en el ojo, lo que le asegurará que se las administró de manera correcta. Si tiene problemas persistentes, como dolor, visión borrosa o dolores de cabeza después de ponerse las gotas, hable con el médico sobre la posibilidad de utilizar otro tipo de colirio. Si desea conocer técnicas adicionales o alternativas, adaptaciones y dispositivos de asistencia que lo ayuden a administrar los medicamentos para el glaucoma, consulte el artículo “Consejos para administrar colirios para el glaucoma (y otros tipos de colirios)”.
- Lávese siempre las manos antes de empezar.
- Incline la cabeza hacia atrás.
- Sujete el frasco boca abajo.
- Sujete el frasco con una mano y colóquelo lo más cerca posible del ojo.
- Tenga cuidado de que la punta del gotero no toque ninguna parte del ojo.
- Con la otra mano, baje el párpado inferior. De esa manera, formará una “bolsa”.
- Administre el número de gotas recetado en la bolsa del párpado inferior. Si utiliza más de un colirio, espere al menos cinco minutos antes de administrar el siguiente.
- Cierre el ojo o aplique una presión ligera sobre el párpado inferior con el dedo durante al menos un minuto. Cualquiera de estos pasos retiene las gotas en el ojo y ayuda a evitar que se drenen en el conducto lagrimal, lo que puede aumentar el riesgo de efectos secundarios.
Cualquiera de estos pasos retiene las gotas en el ojo y ayuda a evitar que se drenen en el conducto lagrimal, lo que puede aumentar el riesgo de efectos secundarios.
El tratamiento con láser
Si los colirios no controlan de manera adecuada al glaucoma, el médico puede considerar el tratamiento con láser como siguiente paso. El tipo de procedimiento láser variará en función del tipo de glaucoma que padezca. En última instancia, el tratamiento con láser reducirá la presión al aumentar el drenaje de líquido del ojo. El procedimiento es breve, casi indoloro y suele realizarse en la consulta del médico con un microscopio específico denominado lámpara de hendidura. En primer lugar, le aplicarán un anestésico en la superficie ocular y utilizarán unas lentes de contacto especiales de gran tamaño para que el médico pueda centrarse en la estructura que necesita tratar con láser. Este láser difiere de la cirugía para errores refractivos de la que puede haber oído hablar, como LASIK y PRK.
Existen varias clases de tratamientos con láser. Cada clase es específica del tipo de glaucoma que se padece: el glaucoma de ángulo cerrado o el glaucoma de ángulo abierto.
La iridotomía periférica láser (IPL)
Este láser crea un pequeño orificio en la parte periférica del iris a fin de proporcionar una vía alternativa de paso del humor acuoso hacia la parte posterior del ojo. Esto permite que el ángulo sea menos estrecho.
La iridoplastia periférica (o gonioplastia)
- Este láser trata una capa del estroma periférico del iris, que en última instancia amplía el sistema de drenaje del ojo. Al hacerlo, el ángulo del ojo será menos estrecho.
La trabeculoplastia láser (TPL)
En este procedimiento, la energía láser se dirige a la red trabecular, que es el sistema de drenaje del ojo. El tratamiento con láser reduce la presión al aumentar el drenaje de líquido del ojo. Se pueden utilizar varios tipos de láseres. Algunos incluyen los siguientes:
- La trabeculoplastia con láser de argón (TLA) se utiliza desde hace más de dos décadas.
- La trabeculoplastia selectiva láser (TSL) es un tratamiento láser más reciente
- La trabeculoplastia con láser de micropulso (TLM) es otro tratamiento láser más reciente.
Los efectos secundarios de todos los tipos de láseres incluyen una inflamación leve del ojo y un posible aumento temporal de la presión. Un tratamiento breve con un esteroide suave o un colirio antiinflamatorio no esteroideo trata cualquier inflamación resultante.
La cirugía
La cirugía para tratar el glaucoma suele ser el último paso para los pacientes que no lograron controlar la presión con colirios ni tratamientos con láser.
En función del tipo de glaucoma y de los factores de riesgo asociados, existen dos tipos básicos de intervenciones quirúrgicas:
- Cirugía filtrante – Trabeculectomía: Durante la trabeculectomía, se realiza una pequeña incisión en la esclerótica (la parte blanca del ojo). El líquido se filtra lentamente por esta incisión hacia una “ampolla”, un espacio cubierto que se crea en la conjuntiva (el tejido fino y transparente que recubre la superficie externa del ojo). El ojo reabsorbe gradualmente el líquido de la ampolla. Esta cirugía proporciona un drenaje alternativo “natural” para que el humor acuoso fluya fuera del ojo.
- Implante de dispositivos de drenaje: El implante de dispositivos de drenaje consiste en insertar de manera parcial un tubo artificial en el ojo. El fluido drena a través del tubo y sale a un recipiente. Esta cirugía proporciona un drenaje alternativo “artificial” con el objetivo de que el humor acuoso fluya fuera del ojo.
Ambos tipos de cirugía demostraron eficacia para reducir la presión ocular. Algunos pacientes pueden seguir necesitando gotas oftálmicas postoperatorias a fin de mantener una presión ocular saludable.
Alternativas quirúrgicas
En los últimos tiempos, se desarrollaron varias opciones quirúrgicas distintas de las mencionadas con anterioridad:
- Implante ExPRESS: Se implanta en el ojo un pequeño dispositivo de acero inoxidable del tamaño de un grano de arroz para drenar el líquido.
- Procedimiento con Trabectome: Se introduce un dispositivo en el ojo a través de una incisión muy pequeña en un extremo de la córnea. Se extirpa una pequeña porción de la red trabecular del ojo, responsable de la salida del líquido, lo que mejora el drenaje. Suele realizarse como parte de la cirugía de cataratas.
- Canaloplastia: Se realiza una incisión en el ojo y se introduce un microcatéter en el sistema de drenaje ocular a fin de favorecer la salida del líquido. Suele realizarse como parte de la cirugía de cataratas.
- Otros procedimientos más recientes se denominan cirugías de glaucoma mínimamente invasivas (CGMI) y atraen mucho la atención de los cirujanos oftalmológicos. El iStent disponible en la actualidad es muy pequeño y se recomienda utilizarlo durante la cirugía de cataratas.
Puede encontrar más información sobre estos procedimientos quirúrgicos en la Glaucoma Research Foundation.
Los tratamientos alternativos, ensayos clínicos e investigaciones
La Glaucoma Research Foundation publicó información sobre tratamientos alternativos para el glaucoma, así como un debate sobre la utilidad de la marihuana medicinal en su tratamiento. La marihuana no se aprobó para el tratamiento del glaucoma debido a su efecto de corta duración en la reducción de la presión intraocular. Sin embargo, existen investigaciones en curso en este campo.
En el campo de estudio del glaucoma muchas investigaciones se están llevando a cobo sobre temas que van desde la identificación de los genes que causan el glaucoma hasta la búsqueda de mejores tratamientos para controlar y vigilar la presión intraocular y proteger el nervio óptico. Puede visitar el National Eye Institute y la Glaucoma Research Foundation para obtener información sobre ensayos clínicos.
Editado por la Dr. Sefy Paulose, marzo de 2022